Surgical Precision
Doctors should be specific when conveying the risk of treatment complications
Complications of medical treatments can be a matter of life or death.
So, understanding risk is of the utmost importance to patients weighing their medical options.
Those patients are best served by their physicians using quantitative rather than qualitative terms to describe the risk of complications, according to a new study by a consortium of researchers at the University of Washington that includes Nidhi Agrawal of the Foster school of Business.

In other words, patients have an easier time drawing accurate conclusions when the risk is presented as a numerical percentage rather than with less precise terms such as “common,” “uncommon” or “rare.” And a specific percentage point estimate is more effective than a range.
“This finding highlights the importance of how risk is communicated to patients if they are to make informed decisions about their care,” says Agrawal, the Michael G. Foster Professor of Marketing at Foster.
Clarifying risk
Agrawal and her co-authors from UW Medicine—Dr. Joshua E. Rosen, Dr. Joshua M. Liao and Dr. David R. Flum—collaborate on research about decision-making at the intersection of business and health. One of the group’s goals is to translate decision-making principles into practice, developing tools and protocols to improve how healthcare providers and patients make decisions.
In this study, 296 participants responded to a series of online surveys that presented the probability of complications associated with two treatment approaches to appendicitis: surgery or a course of antibiotics.
The probability of a particular complication was described with:
- a simple percentage (“a 3% risk,” for example),
- a range of percentages (“a 1% to 5% chance”), or
- a verbal descriptor (such as “common,” “uncommon” or “rare”).
The respondents were then asked to estimate the likelihood of a complication for a typical patient with appendicitis by using a sliding scale that ran from 0 to 100%.
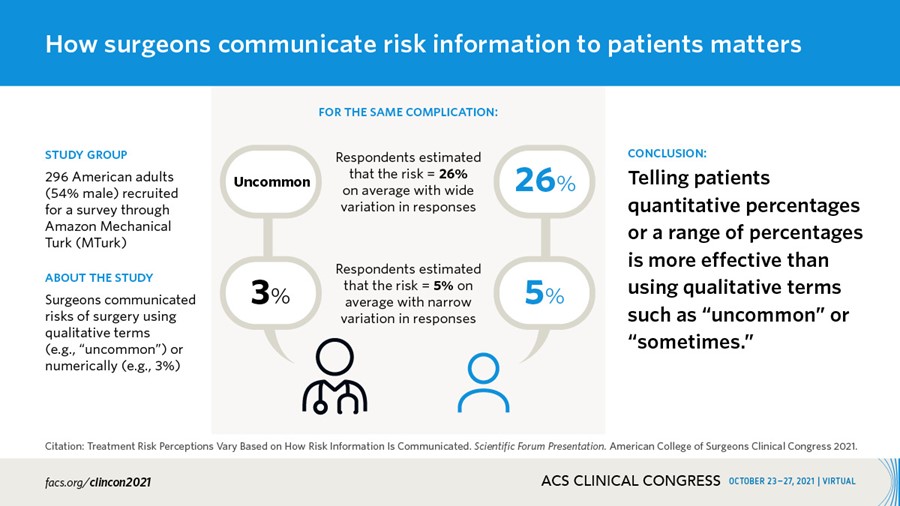
The perception of risk among those who had been given the probability as a simple percentage tended to be in much closer agreement than those who had the risk conveyed with a verbal descriptor. For example, when the risk of diarrhea with antibiotic treatment was described as “common,” the majority of participants interpreted the risk as being anywhere from 39% to 84%, while those who were told the risk was “7%” or a “range of 5% to 9%” showed much less variation in their estimates.
More informed decisions
Dr. Rosen explains that physicians use verbal descriptors to express risk for a variety of reasons. For one, they may want to put patients at ease by not overwhelming them with numbers. Or they may not have numerical estimates quickly available on a busy call shift.
“It’s a common concern that patients won’t understand numerical information,” he says. “But the participants in our study did well with both percentages and ranges. It’s a signal that patients, too, can work with the numbers we give them.”
Based on the study’s insights, the researchers plan to develop tools—such as handouts and decision aids—to help healthcare providers convey risk information to patients more effectively.
This work is part of a broader portfolio through the UW Value and Systems Science Lab and Decision Science Group that seeks to foster collaboration across disciplines and improve the way that doctors, clinical teams, patients and their loved ones make healthcare decisions.
“Treatment Risk Perceptions Vary Based on How Risk Information Is Communicated” was presented to the 2021 American College of Surgeons Clinical Congress.